The Hidden Cost of Misplaced ECG Leads in Emergency Care
Every day in emergency departments and ambulances across the country, medical professionals place ECG electrodes on patients. It's such a routine procedure that few stop to question whether they're doing it correctly. But research reveals a startling truth: the majority of healthcare providers—from nurses to cardiologists—are placing these critical diagnostic sensors incorrectly.
The Scope of the Problem
Multiple peer-reviewed studies have documented the widespread nature of electrode misplacement:
These aren't isolated incidents or the result of inadequate training. They represent a systemic challenge inherent in the traditional approach to ECG electrode placement—one that persists despite decades of emphasis on accuracy in medical education.
The Clinical Consequences
When electrodes are misplaced, the consequences extend far beyond technical inaccuracy. They create a cascade of clinical challenges:
1. False-Positive Diagnoses
Misplaced V1 and V2 leads can create the appearance of anterior ST elevation, potentially triggering emergency cardiac catheterization for patients who aren't actually experiencing a heart attack. This exposes patients to unnecessary risk and costs healthcare systems thousands of dollars per false activation.
2. Missed Critical Diagnoses
When limb leads are placed on the torso instead of extremities—a common shortcut in busy pre-hospital settings—inferior wall infarcts can be completely hidden. This delay in diagnosis can mean the difference between full recovery and permanent cardiac damage.
3. Inconsistent Baseline Comparisons
When an EMS provider uses one electrode placement technique in the field and the emergency department uses another, comparing the two ECGs becomes problematic. Changes between tracings might reflect differences in technique rather than actual changes in the patient's cardiac status.
4. Training and Quality Assurance Challenges
EMS agencies and hospitals spend significant resources training staff on proper electrode placement, yet accuracy remains elusive. Quality assurance programs struggle to effectively monitor and correct placement errors in real-world, time-pressured environments.
Why Traditional Methods Fail
The root cause isn't lack of knowledge or effort. Traditional electrode placement requires:
Even experienced clinicians face challenges with patient factors like obesity, unusual chest wall anatomy, breast tissue, and the urgent nature of many ECG acquisitions.
The Cost Beyond Dollars
While misplaced electrodes certainly carry financial costs—in unnecessary procedures, extended diagnostics, and quality improvement initiatives—the human cost is more significant:
The Solution: Systematic Rather Than Individual
For decades, the healthcare industry has approached electrode misplacement as an education and training problem. But perhaps it's actually a design problem.
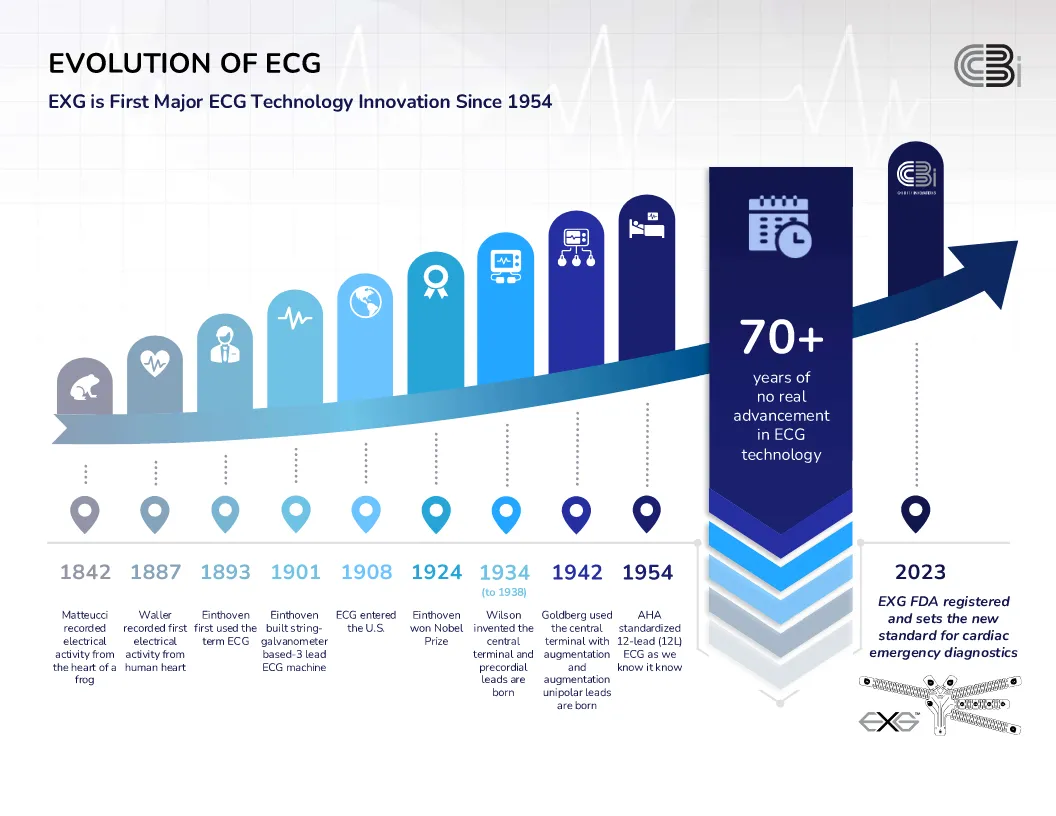
The EXG™ Radiolucent Electrode System represents a paradigm shift: instead of trying to improve how clinicians place individual electrodes, it eliminates the need for individual placement decisions entirely. By integrating all 10 electrode sites into a single device with clear anatomical alignment markers, it makes accurate placement the default rather than the exception.
Evidence of Impact
Early adoption of the EXG™ system in EMS agencies and emergency departments has demonstrated:
The Bottom Line: Electrode misplacement isn't a failure of individual clinicians—it's a systemic challenge requiring a systemic solution. The EXG™ system represents that solution, transforming 50-year-old technology to meet the demands of modern emergency medicine.
