Frequently Asked Questions
CBI EXG FAQ 2026 - Find answers to common questions about the EXG Wearable ECG Platform
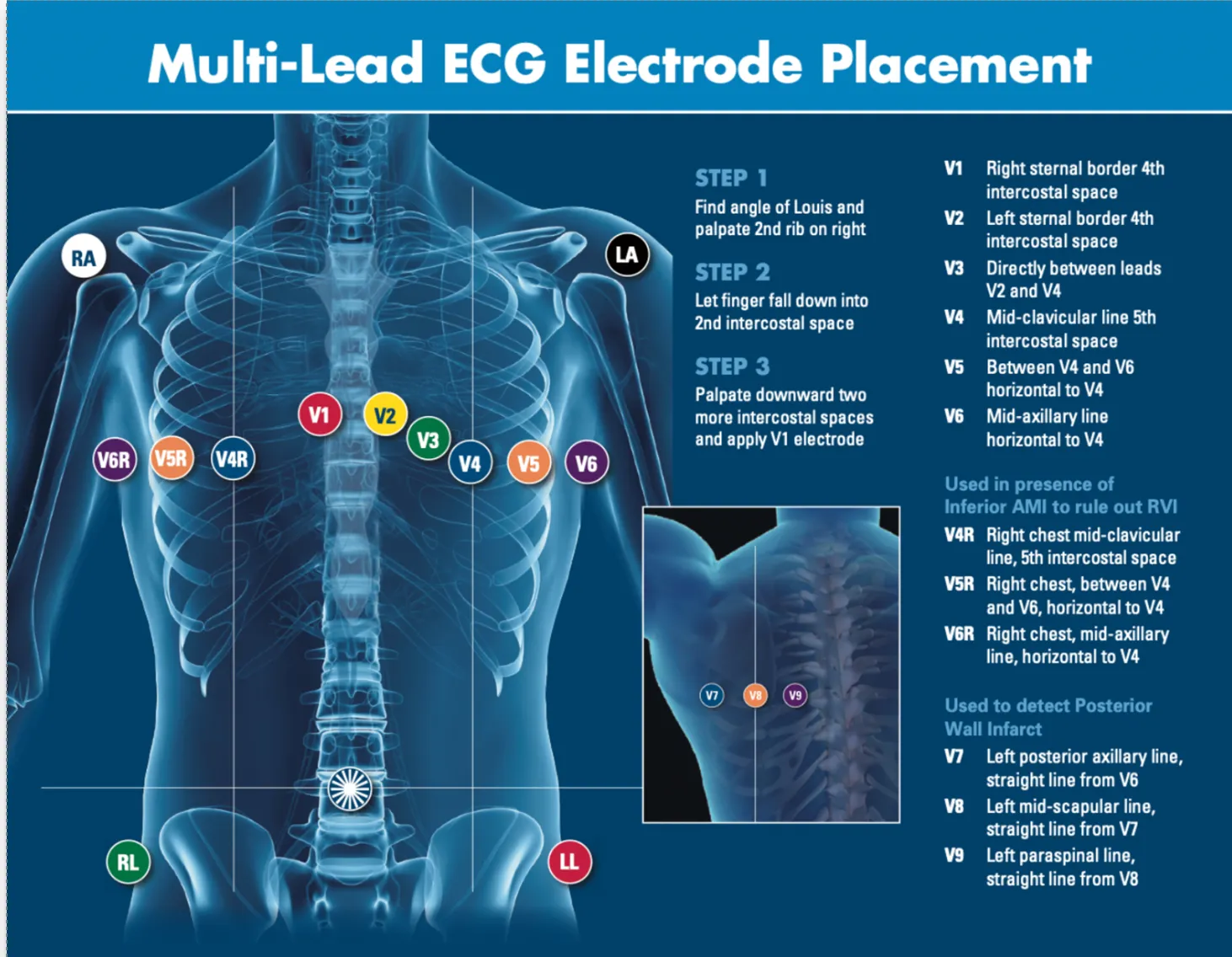
ECG Electrode Placement Guide
Proper electrode placement is critical for accurate ECG readings. The EXG system's intuitive design ensures consistent, AHA-compliant positioning every time, eliminating the guesswork from traditional lead placement.
- ✓Anatomical landmarks for precise positioning
- ✓Color-coded leads for quick identification
- ✓Works across all patient body types
Frequently Asked Questions
Find answers to common questions about the EXG platform
EXG is an FDA-registered, radiolucent wearable 12- to 18-Lead continuous diagnostic ECG (electrocardiogram) system now in use across EMS and hospital settings to improve the detection of cardiac emergencies. The EXG Radiolucent Electrode System is indicated for use by healthcare professionals for ECG monitoring. The EXG 12-Lead device is disposable for single use and has been tested for up to 72-hour wear. The EXG Radiolucent Electrode System consists of a 12-Lead Electrode and an optional 3-Lead Posterior and Right Sided ECG Electrode. - EXG supports pre-hospital to in-hospital fast transitions and continuity of care - EXG promotes equity in care by simplifying ECG for all users and body types - EXG shaves minutes off ECG acquisition and repeat acquisition, doesn't delay scene time - Ensures proper ECG placement every time with its intuitive design The EXG system also consists of single use 4-Lead and 5-Lead wearables for use in low-acuity situations for heart rate and rhythm analysis. All of the EXG systems use the same universal single cable enabling connectivity to all pre-hospital (Zoll, Stryker) and in-hospital monitoring systems (e.g., GE, Nihon Koden, Philips).
Key benefits of EXG vs. traditional electrodes include: Speed of Application: EXG is applied in 20-30 seconds, enabling rapid diagnosis. Traditional lead-by-lead placement takes up to 3-5 minutes. Length of Wear: EXG is validated for 3-day wear allowing seamless integration into the inpatient setting as the monitoring electrode. Traditional electrodes require multiple different forms during a hospital stay adding complexity and cost. Accuracy & Consistency: EXG ensures proper placement every time with intuitive design with 100% improvement in electrode placement. Up to 90% of traditional ECGs contain errors due to lead misplacement. Tolerates CPR: EXG tolerates mechanical and manual CPR with ability to acquire post ROSC 12-Lead ECG in seconds. Traditional electrodes are not compatible with CPR. Repeat ECGs: EXG takes seconds to re-acquire without removing and reapplying leads. Traditional electrodes require full reapplication, delaying reassessment. Skin Contact & Signal: EXG provides improved skin impedance for high-fidelity ECG signals. Traditional electrodes have variable contact that can cause poor signal quality. Radiolucency: EXG can remain in place during X-ray, CT, Cath Lab, and EP procedures. Traditional electrodes must be removed or repositioned, interrupting workflow. Patient Safety: EXG has potential to reduce false positives/negatives, helping guide accurate decisions. Traditional electrode errors lead to misclassification and treatment delays. Integration: EXG has universal compatibility. One cable fits any ECG monitor/defib (pre-hospital and hospital monitors), supports serial ECGs and monitoring. Traditional electrodes need multiple cables and snap-ons, increasing complexity. Stress Test Lab: EXG can be worn for exercise treadmill stress testing with no modifications. Traditional technology is cumbersome and frequently introduces noise and errors. EMS-to-ED Transition: EXG provides seamless handoff with no need to rewire or reposition. Traditional electrodes require new acquisition in the ED, delaying treatment.
- Misapplication of electrodes by only inches can obscure and hide a heart attack - 2% increase in mortality for every 1-minute delay in STEMI diagnosis - 2% decrease in ejection fraction for every 1-minute delay in STEMI diagnosis and treatment
We appreciate that this conversation can be an uncomfortable conversation to have as some paramedics/EMTs who may believe that "it doesn't happen here". The reality is that, while on an individual level some medics may consistently place leads correctly, the majority do not. If they place leads incorrectly, there is no inherent traceability in the system other than limb lead transposition. Additionally, medics fail to skin prep or place the patient in a supine position to take the initial or serial ECG. Paramedics and EMTs are consistently placing ECG leads incorrectly. This is supported by research, and healthcare providers are aware of this persistent issue. Studies confirm that technical errors have significant consequences for patient diagnosis and treatment. Multiple studies have found a high level of inaccuracy in the placement of ECG leads by emergency medical services (EMS) personnel: - A 2024 study on EMS personnel showed significant variation in chest electrode placement, with only 41.6% rated as "acceptable" on a mannequin. - Research cited in a 2024 article revealed that as few as 5.8% to 41.6% of paramedics placed all electrodes correctly on manikins. - A 2019 study on UK paramedics found that only 5.8% of participants could accurately place all chest leads, confirming a high degree of variation. - These inaccuracies are not limited to EMS. Research has also shown frequent misplacement among nurses and even cardiologists. Several factors contribute to persistent placement errors by EMTs and paramedics: - Lack of continuous training: ECG refresher training does not always occur annually for paramedics/EMTs. - Patient factors: Obese patients, those with large breasts, or people with excessive hair can make it challenging to find the correct anatomical landmarks. A tendency to place electrodes incorrectly above and below the bra on female patients leads to misplacement. - Time pressure: In emergency situations, speed is prioritized, and the high cognitive load during emergency situations leads to shortcuts like placing leads without locating landmarks accurately. - Poor feedback loops: Historically, there has been a lack of consistent feedback from hospitals to EMS crews regarding the accuracy of their ECGs. Some regions have addressed this with data-sharing agreements, but it is not universal. Additionally, the monitors themselves only provide limited awareness of lead misplacement (e.g. limb lead reversal). - Failure to recognize standards: Patient positioning affects ECG analysis. Seated and upright ECG acquisition can lead to inaccurate algorithm performance because the heart moves forward during repositioning. The algorithms used to detect heart attacks were designed to be used with patients in a supine position. Common errors in lead placement include: - V1 and V2 leads are too high: The most common error is placing the V1 and V2 electrodes one or two intercostal spaces too high on the chest. Systematic errors in this placement often occurs in females. The hesitancy to remove bras and coverings to expose the breasts to ensure proper positioning can decrease detection of anterior STEMI by 11% - Limb leads on the torso: In pre-hospital settings, it is common to see limb leads placed on the chest or abdomen to save time and reduce movement artifact during patient transport. - Other precordial errors: Other misplacements include V4 being too low and to the left, V5 below its expected position, and various other vertical and horizontal displacements. Consequences of misplacement: - Hiding a heart attack: Superiorly misplaced V1 and V2 leads can HIDE anterior STEMI criteria and create a false-negative reading for a ST-segment elevation myocardial infarction (STEMI). Placing limb leads on the torso can HIDE an inferior-wall myocardial infarction, causing a life-threatening condition to be missed. - False changes in condition: When an inaccurate ECG is followed by a correct one at the hospital, the differences in the readings may be misinterpreted as a change in the patient's medical condition. False positive and false negatives can occur with changes in positions. False STEMI activations are often caused by electrode misplacement. EXG's anatomical landmarks and intuitive design enable consistent accurate placement.
Yes! Our clinical validation studies show that the use of the EXG alone is at least 2 minutes faster than traditional leads when measuring head-to-head EXG versus ECG placement among medics. When introduced into an EMS system where proper patient positioning, skin prep and exposure were introduced, FMC to ECG decreased by 1 minute, and the number of uninterpretable ECGs decreased from over 7% to 3%, and the overall quality improved!
Yes! The EXG Radiolucent Electrode System is indicated for use by healthcare professionals for ECG monitoring in patients. The flexible lattice designed limb leads and V4-V6 leads can be stretched or compressed to accommodate different body types, both small and large. EXG has been designed to accommodate up to 95% of the patient population (i.e., greater than 500 lbs.).
The 4-Lead EXG electrode system was developed for cardiac monitoring in patients that are not suspected of having acute coronary syndrome, but where cardiac monitoring is desired. The 4-Lead EXG electrode system can be applied in several configurations including wrist-to-wrist, wrist to chest, etc.
Yes. EXG has been designed to allow removal and replacement if you are not satisfied with its initial placement. Traditional electrodes tend to lose adhesive strength after reapplication.
No. The 3-Lead, 4-Lead, 5-Lead, and 12-Lead EXG electrode systems have been designed for single use only.
Yes. EXG has passed biocompatibility testing for cytotoxicity, skin sensitization and irritation. The product does not contain latex.
Yes, the EXG devices are radiolucent and will not interfere with catheterization procedures.
Currently, the EXG radiolucent electrode system has a 2-year shelf life from its manufacturing date.
Yes. However, as with all electrodes, it is necessary to first remove off the sweat and moisture. The quick application of EXG ensures it can be applied to dry skin and once on, will tolerate sweating and diaphoresis.
Yes. EXG is compatible via the universal EXG snap adapter with all cardiac monitors. The EXG single cable design connects to the snap adapter which connects to the monitor cable contained within the portable monitor bag or connected to the hospital monitor. The one-time, "set it and forget it" design enables our single cable to be connected to the monitor directly to the patient so the previously used 4-Lead or 10-lead cable are no longer needed.
The EXG single cable design connects to the snap adapter which connects to the monitor cable contained within the portable monitor bag or connected to the hospital monitor. The one-time, "set it and forget it" design enables our single cable to be connected to the monitor directly to the patient so the previously used 4-Lead or 10-lead cable are no longer needed. This frees up space in your bag.
Yes! The EXG packaging and wearable design does allow folding over of the packaging so several units can be stored in the pre-hospital monitor bags.
No. The EXG 12L is designed to stay on the patient for fast, seamless transitions into the hospital. If the hospital is also an EXG user, the pre-hospital provider can just unclip the EXG system as they transition the patient to the in-hospital monitor. The 12L wearable is indicated for 3-days of use and can travel with the patient from the ED to the cath lab and into in-patient facilities.
Yes. The EXG 12L can be placed on a patient that is undergoing CPR. The EXG 12L can be placed on a patient during a pulse check and compression can continue. The EXG 12L can be used under manual or automated compression. When using anterior-apical defibrillation pads it is possible for the pad to overlap the V1 electrode. In such cases, we recommend shifting the V1 electrode medially to avoid interference with the defibrillation pad. To accommodate anterior posterior pad placement, the anterior pad can be placed below the V3-V6 strip and the posterior pad beside the scapula. This ensures both effective defibrillation and accurate ECG readings.
Yes. However, when the patient is over 400 - 500 lbs. diagnostic ECG capabilities for all electrodes and monitors are diminished. For a patient that exceeds these weights, you are only able to get accurate rate and rhythm by using the EXG 3L electrode with the 12L for placement of V6.
All electrodes recommend skin prep to improve the fidelity of ECG tracings, including EXG. Skin prep can be easily performed with EXG prior to during application without increasing FMC-to-electrode or scene time.
Still Have Questions?
Our clinical specialists are here to help answer any questions about the EXG platform
