EXG Clinical Study
In-field clinical study of the EXG 12-Lead Electrode System demonstrating improved ECG acquisition speed and signal quality in real-world EMS settings
Saint Louis Community Fire Protection District, MO (299 Patients)
February 14, 2025 – June 30, 2025
March 1, 2024 – June 30, 2024
Stryker LIFEPAK 15
EXG Clinical Study
Background: Electrocardiogram (ECG) accuracy is critical for timely cardiac care. Yet in the prehospital setting, ECG acquisition lacks adherence to AHA guidelines such as full chest exposure, skin preparation, supine positioning, and precise lead placement. The EXG radiolucent electrode system was developed to address these compliance gaps by standardizing ECG application and improving diagnostic workflow.
Methods: We conducted a study within the St. Louis Community Fire District, comparing patients with chest pain or rhythm disturbances managed with the EXG system to a historical cohort using conventional Ambu® BlueSensor electrodes.
Results: Among 299 patients, EXG use was associated with a shorter median time from first medical contact (FMC) to ECG (6 minutes vs. 7 minutes), fewer uninterpretable ECGs (3.2% vs. 7.2%), and more clean tracings (OR 1.88). EXG was not independently associated with prolonged scene times.
Download Full Study
Access the complete In-Field clinical study including methodology, detailed results, statistical analysis, and conclusions.
Download PDF StudyKey Findings
Median time from first-medical-contact (FMC) to ECG (6 min vs 8 min)
Reduction in uninterpretable ECGs (3.2% vs 7.2%)
Odds ratio for clean ECG tracings with EXG system
Study Figures
Visual data from the clinical study
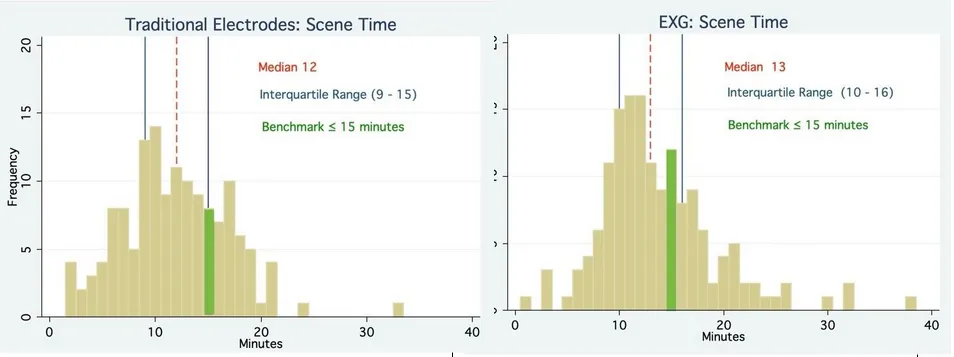
Figure 1: Scene Time Distribution
Histograms comparing scene time (minutes) by electrode type, showing distribution patterns for both EXG and traditional electrodes.
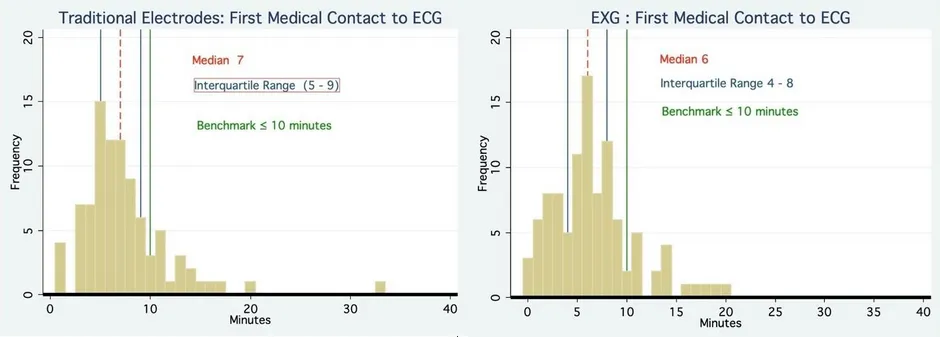
Figure 3: Multivariable Analysis
Forest plot showing odds ratios for factors associated with benchmark scene time, demonstrating EXG is not associated with prolonged scene times.
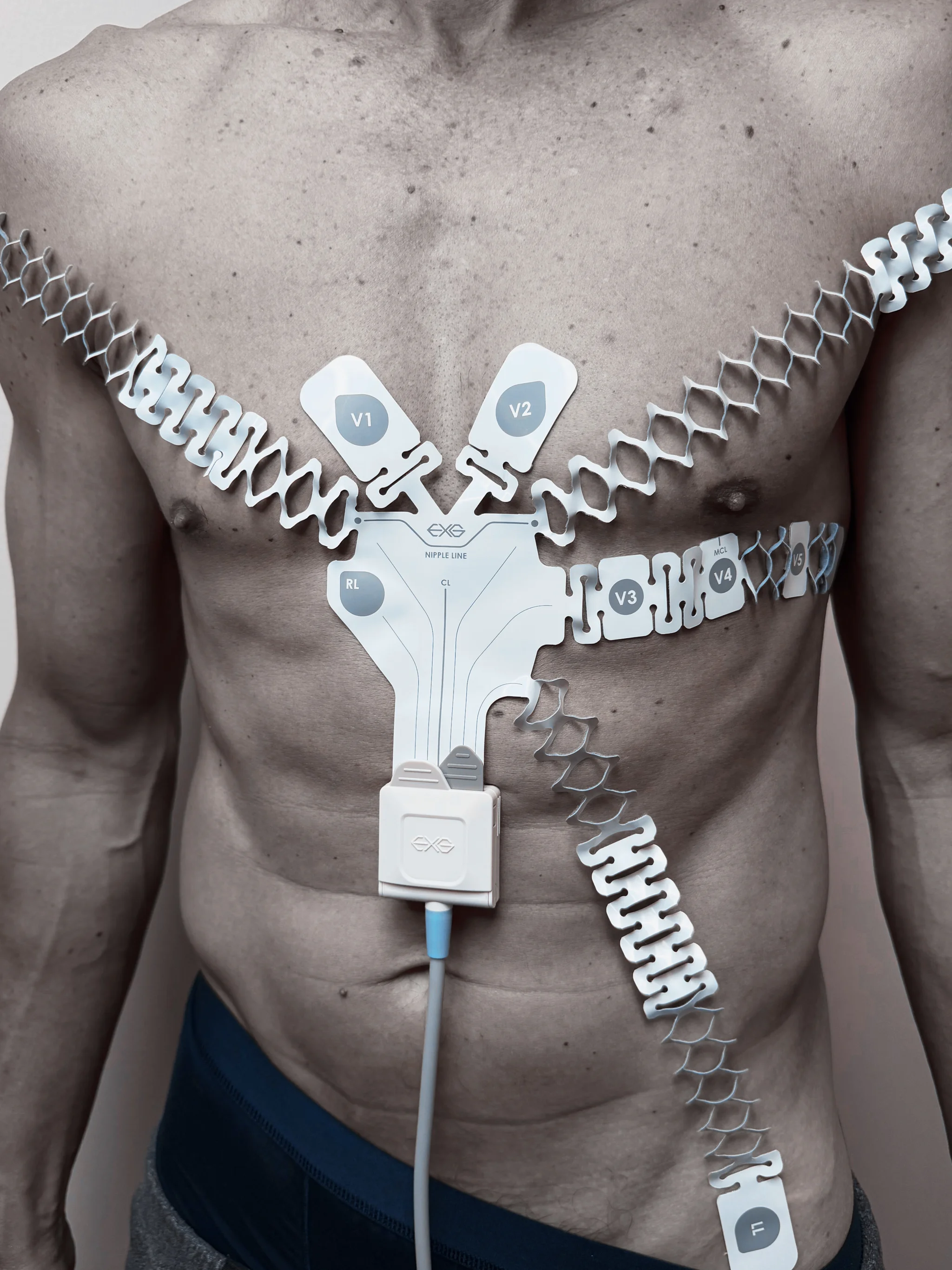
Reinforced AHA Guidelines
EXG applied with patient supine, skin abraded beneath each electrode, and correctly positioned using indexed anatomical markers for guideline-concordant ECG acquisition.
- Full chest exposure with proper skin preparation
- Supine patient positioning per AHA guidelines
- Indexed anatomical markers for precise placement
Conclusions
Compared to conventional electrode application often performed over clothing and without skin prep, the EXG electrode system enabled more accurate electrode placement without delaying scene time.
Study Authors
Christian McClung MD MPhil, AJ Naha BA, Stephen Dunphy MD, Chris Meier BC/CMO, Justin Rapoff MD
Learn More About EXG Clinical Evidence
Request detailed clinical data or schedule a demonstration of the EXG™ platform
